Consults

Just as with many aspects of health, when there are no symptoms and all seems well, it can become easy to take eyesight for granted. It may be surprising to hear that most forms of vision loss are either preventable or treatable but unfortunately some eye conditions are insidious – causing no obvious symptoms until they become advanced.
From the age of 40, it is normal to experience changes in your vision. Your risk of developing certain eye conditions also starts to increase. We recommend that you have regular eye tests with your optometrist to ensure any issues are detected as early as possible.
Nelson Eye Surgeons treat a wide variety of eye conditions and also perform cataract surgery. We have completed extensive post-graduate specialist training in order to become general ophthalmologists. In addition, we have also undertaken further training and extra qualifications in specific diseases or conditions affecting the eye – this is called subspecialisation.
This is a full evaluation of the front, middle and back of the eye, focusing on the issues of concern and includes an assessment of vision, pupils, eye pressure, anterior segment, retina, and optic nerve and select diagnostic tests. In certain circumstances this may be accomplished through virtual eye care.

Preliminary Eye Assessment:
- Vision Measurement
You will read an eye chart to determine how well you see at various distances. You cover one eye while the other is being tested. This exam will determine your best vision with and without glasses (whether you have 20/20 vision or not). - Pupils
The technician will check how your pupils respond to light by shining a bright beam of light into your eye. Pupils usually respond by getting smaller. - Auto-refraction
This is a measurement that estimates what strength of glasses you may require to correct your vision. - Eye pressure (intraocular pressure) measurement
Eye pressure testing, or tonometry, measures the pressure within your eye (intraocular pressure or IOP). Elevated IOP is a sign of glaucoma. You will receive a numbing drop on the eye to improve comfort when testing. - Other specialised tests may include: colour vision test, Amsler grid, tear film testing.
Diagnostic tests at the time of your visit may include:
- OCT test
Cross sectional image of the back of the eye – retina and optic nerve. - Pachymetry test
Measurement of thickness of the cornea at the front of the eye. - Anterior chamber angle testing
OCT picture and gonioscopy measurement of the angle between the cornea and the iris at the front of the eye. - Visual field test
Peripheral or side vision test.
After our ophthalmic technician or nurse completes the pre-assessment and diagnostic tests, you may then have drops instilled into the eyes, which open up the pupils (dilating drops) and allows for a more complete assessment of the deeper structures of the eye, including the retina and optic nerves.
Once the dilating drops have worked (on average 20-30 minutes after instillation) you will then be directed to one of the clinic rooms, where you will see the eye doctor (ophthalmologist).
Examination with an Ophthalmologist
The ophthalmologist will meet with you and will confirm why you have come for your visit today. She or he will then review your eye history, medical history and medications, allergies. You may be asked to repeat a few questions which you have answered previously. The doctor will review any forms which you completed earlier during your visit and will also review other documentation including doctor reports, test results, diagnostic tests (OCT, pachymetry, angle measurement, visual field test, IOL master, and/or topography). Testing done outside of the office may also be reviewed and discussed if available/applicable.
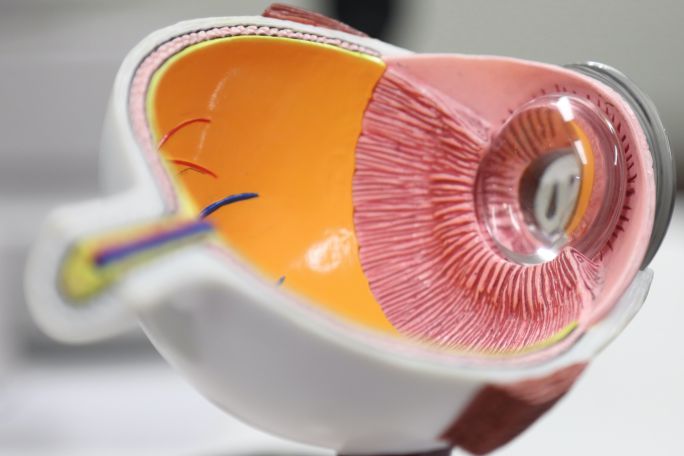
Your eyes will then be examined by the ophthalmologist. The examination will include a slit lamp examination (a microscope mounted on a table) in order to see the “anterior segment” or front part of the eye (the eyelids, the cornea, the iris, the angle, the lens and other structures) and the back of the eye (including the retina and the optic nerve). The ophthalmologist may also use an indirect ophthalmoscope (headset) to view the retina and optic nerve.
If required, you may have a test involving a mirror-lens that is placed on the surface of the eye (after numbing drops are instilled), in order to check more details at the front and back of the eye.
Other tests may involve eye movement testing, eye muscle balance testing, pupil testing and measurement of eyelid opening and movement.
